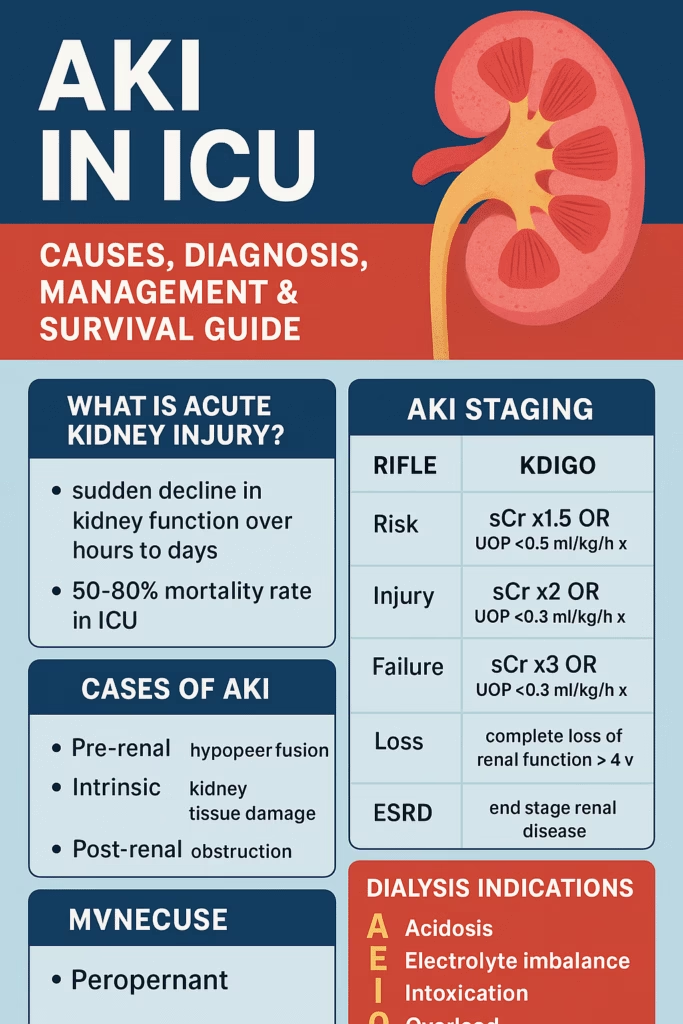
🩺 AKI in ICU: Causes, Diagnosis, Management & Survival Guide (Complete 2025 Updated Post)
Author: Dr Sanjay Prajapati
Category: Critical Care | Nephrology
Reading Time: 8 minutes🩺 AKI Acute Kidney Injury in ICU: Causes, Diagnosis, Management & Survival Guide (Complete 2025 Updated Post)
🔍 Overview
Acute Kidney Injury (AKI) in ICU patients is a life-threatening emergency with high mortality. Learn causes, KDIGO staging, diagnosis, management, dialysis indications, and prevention in this complete ICU guide.
🧠 What is Acute Kidney Injury (AKI)?
Acute Kidney Injury (AKI) is a sudden decline in kidney function over hours to days.
It is extremely common in ICU patients and has a 50–80% mortality rate.
📌 KDIGO Definition of AKI
AKI is diagnosed if any of the following occur:
- Increase in serum creatinine ≥ 0.3 mg/dL within 48 hours
- Increase ≥ 1.5 × baseline within 7 days
- Urine output < 0.5 mL/kg/hour for 6 hours
Important: Criteria should be applied only after optimizing fluid status.
🚦 AKI Staging (RIFLE, AKIN, KDIGO)
🔥 RIFLE Criteria
| Stage | Creatinine | Urine Output |
|---|---|---|
| Risk | 1.5× baseline | <0.5 mL/kg/hr × 6 hrs |
| Injury | 2× baseline | <0.5 mL/kg/hr × 12 hrs |
| Failure | 3× baseline | <0.3 mL/kg/hr × 24 hrs |
| Loss | Renal failure > 4 weeks | |
| ESRD | End-stage kidney disease |
🔥 AKIN Criteria
- Stage 1: 1.5× Cr or +0.3 mg/dL
- Stage 2: 2× Cr
- Stage 3: 3× Cr, Cr >4 mg/dL, or dialysis needed
🩸 Why Serum Creatinine Is Not Reliable Alone
- It lags behind injury
- eGFR formulas do NOT apply in AKI
- Affected by muscle mass, hydration, and distribution volume
⚠️ Causes of AKI (Prerenal, Intrinsic, Postrenal)
1️⃣ Prerenal (Most Common in ICU — Hypoperfusion)
- Volume loss (diarrhea, vomiting, hemorrhage)
- Hypotension
- Heart failure
- NSAIDs
- Contrast-induced AKI
- Hepatorenal syndrome
2️⃣ Intrinsic AKI
- ATN (Acute Tubular Necrosis) – ischemia, sepsis, drugs
- Glomerular: GN, Goodpasture
- Interstitial: drug allergy, pyelonephritis
- Vascular: renal artery stenosis, emboli
3️⃣ Postrenal (Obstruction)
- Prostate enlargement (BPH)
- Bilateral stones
- Tumors
- Neurogenic bladder
- Retroperitoneal fibrosis
🧪 Diagnosis & Workup in AKI
🔹 History & Examination
Check for:
- New medications
- Fluid loss
- Heart failure signs
- Edema, JVD
- Bladder distension
- CVA tenderness
🔹 Key Investigations
- BUN, Creatinine
- ABG, Electrolytes
- CBC
- Serology: ANA, ANCA, HBV, HCV, anti-GBM
🧫 Urinalysis Clues (Very Important for Differentiation)
Prerenal AKI
- Bland urine
- High osmolality
- Low Na (<20 mEq/L)
- FeNa <1%
Intrinsic AKI (ATN)
- Muddy brown casts
- Na >40
- FeNa >2%
- Osm <350
🖥️ Ultrasound Findings
- Hydronephrosis → obstruction
- Small kidneys → chronic disease
- Normal size → acute process
🏥 AKI in ICU: Why More Dangerous?
Incidence in ICU: 40–60%
Mortality: >50%
Risk Factors
- Age
- Sepsis
- Liver disease
- Heart failure
- Mechanical ventilation
💉 Management of AKI in ICU
1️⃣ General Principles
- Treat underlying cause
- Maintain MAP > 60 mmHg
- Avoid nephrotoxic drugs
- Optimize fluids
- Track I/O, weight, BP
- Correct electrolytes
💊 Dialysis Indications — AEIOU (Life-Saving Rule)
| Letter | Indication |
|---|---|
| A | Acidosis (pH < 7.1) |
| E | Electrolyte imbalance (K+ > 6.5) |
| I | Intoxication (SLIME drugs) |
| O | Overload (pulmonary edema) |
| U | Uremia (pericarditis, encephalopathy) |
🛠️ Dialysis Modalities
🌀 Intermittent Hemodialysis (IHD)
- Fast removal
- Best for small molecules
💧 CRRT (Continuous Renal Replacement Therapy)
- Gentle
- Ideal for unstable patients
- Less hypotension
🫧 Peritoneal Dialysis
- Alternative when others unavailable
🔄 Stopping Dialysis
Stop when:
- Urine output improves
- Creatinine starts declining
- Creatinine clearance rises
🛡️ Prevention of AKI
Non-Drug
- Hydration
- Maintain MAP
- Avoid nephrotoxins
Drug-Based
- Diuretics
- Mannitol
- Fenoldopam
- Natriuretic peptides
🧭 Prognosis
- Mortality >50% with multiorgan failure
- Many recover, but some develop chronic kidney disease
- Prevention is the key to survival
❓ Frequently Asked Questions (FAQ)
Decreased urine output is the earliest warning sign.
Yes — especially prerenal AKI, if treated early.
Use the AEIOU criteria.
Yes, nearly 40–60% of ICU patients develop AKI.